Twenty four hours from now I sure as shit better be in a room on the surgical floor. It is mid-evening on Wednesday, the operating room is reserved for me from 7:30 AM to 1 PM tomorrow. For some unclear reason, I need to be at the hospital at 6:00 AM so we have a nanny coming at 5:30 AM to the house.
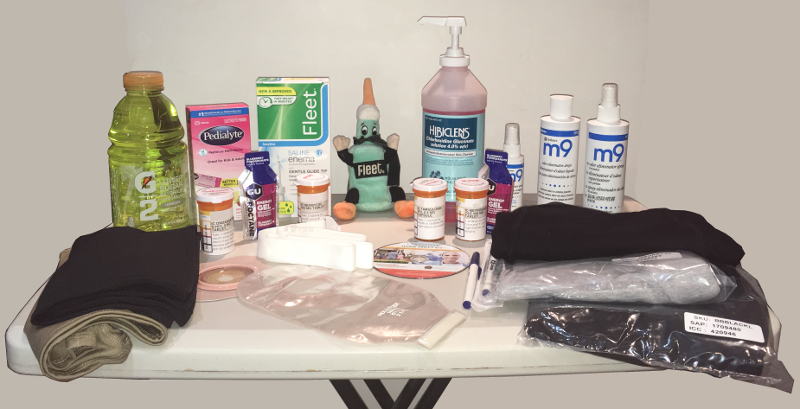
I made an error in my photo in the last post as to my preparations. I do not need to take any enema today! But I need to drink two bottles of magnesium citrate, one at noon and one four hours later. I need to take a lot of antibiotics today, and am into that process. The last two days, and today, I am taking a pill that relaxes the neck of my bladder. Apparently when a male has surgery in their pelvic area it is often hard to urinate for a few days. In an effort to not need a catheter, they use this pill as part of the preparation. Trust me, if I need a catheter, you will know …
I have spent the last few hours making many trips to the toilet. The inside of my colon, I am sure, is bright and shiny right now. My stomach is not so great from the antibiotics, and there are more to come. I still need to take my shower with the surgical scrub, tonight and tomorrow.
I think I am set. I have very high confidence that I will wake up from surgery, I have every time in the past. That is the next milestone, followed by getting my butt back home, hopefully by Monday. That depends on my stoma working well and my working well with the stoma. We are going to be dear friends.
Inanna is incredible. My mom traveled to here and my sister lives here. Being co-chair of an organization whose membership is overwhelmingly women caregivers is helpful! And we have some wonderful nannies (our word for the personal care attendants) working with the girls.
I am not scared, because there is nothing tomorrow to be scared about. I am anxious about the pathology report but that will be days away. I have come to terms with the stoma, and I am practicing to make a good first impression with it. I hope it likes me.



4 comments on this ↑ post, add yours (or read theirs)