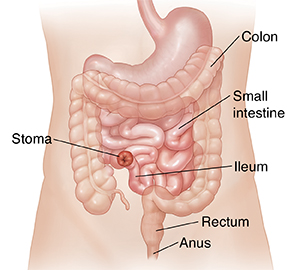
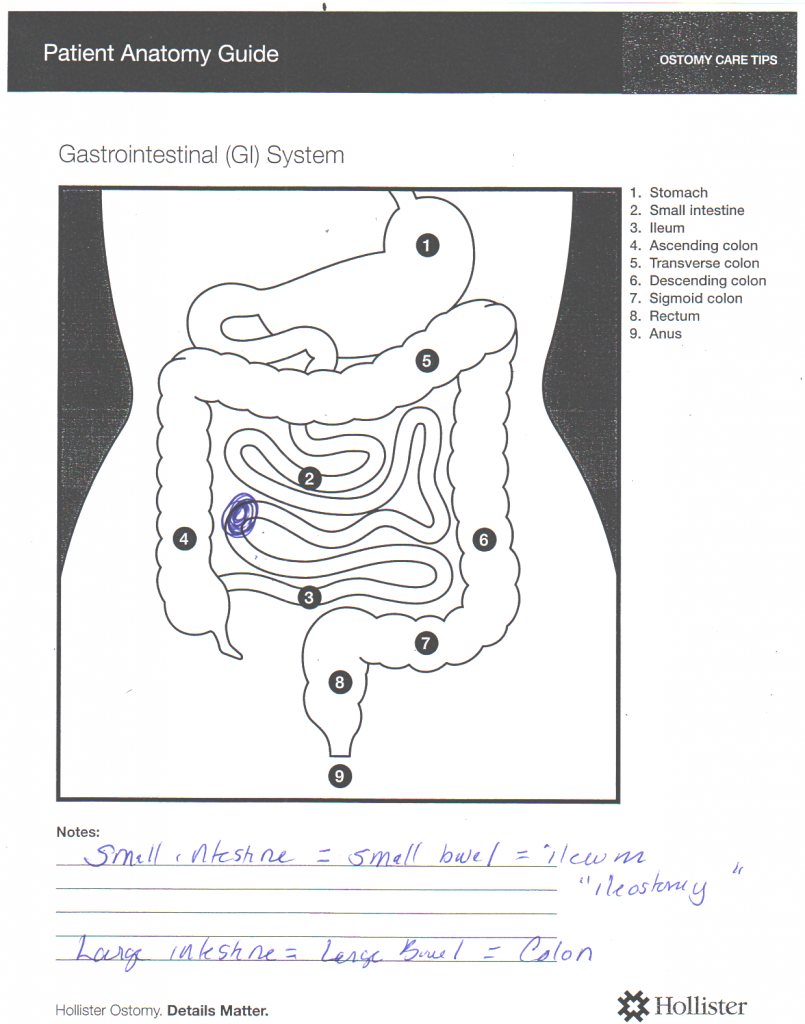
First, a follow-up to the previous post. I found a great video that shows, via animation, all about the ileostomy. There are no disturbing true-life images! It was written for patients with irritable bowel disease (IBD) since they also often need an ileostomy but all the information is the same.
Now the question is, how the hell are they going to get the cancer out of me? As far as I am concerned, since the doctor can feel the tumor with his finger in my butt, why don’t they just take it out that way? I don’t know, but truthfully, I don’t want to know.
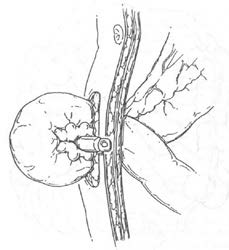
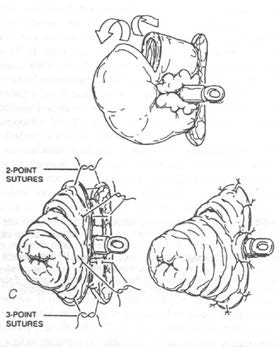
In the past, a surgeon would cut open my abdomen, through skin, muscle, and yuck; retractors would hold the foot long incision open, and they would dig around, take out part of my colon, etc. That has now gone the way of leeches I guess (although leeches still have a place in medicine) and the surgery is done laparoscopically.
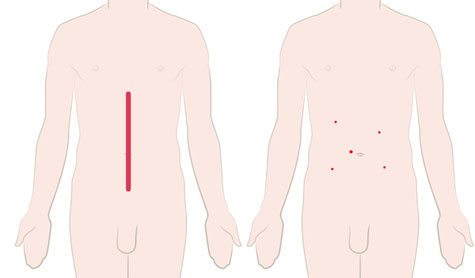
This shows the difference in surgical openings:
Click here to see an actual photographic comparison
 “Open and laparoscopic abdominal incisions after urgent total abdominal colectomy for CUC. Left panel: laparotomy with staples; right panel: laparoscopic subtotal colectomy with one 12-cm port site hidden in the diverting stoma, three 5-mm suprapubic, and 1 left lower quadrant ports are imperceptible. Left panel courtesy of Holubar; Right panel courtesy of Dozois, May Clinic, Rochester.” From here.
“Open and laparoscopic abdominal incisions after urgent total abdominal colectomy for CUC. Left panel: laparotomy with staples; right panel: laparoscopic subtotal colectomy with one 12-cm port site hidden in the diverting stoma, three 5-mm suprapubic, and 1 left lower quadrant ports are imperceptible. Left panel courtesy of Holubar; Right panel courtesy of Dozois, May Clinic, Rochester.” From here.
Laparoscopic surgery, also called minimally invasive surgery (MIS), bandaid surgery, or keyhole surgery, is a modern surgical technique in which operations are performed through small incisions (usually 0.5–1.5 cm) elsewhere in the body.
There are a number of advantages to the patient with laparoscopic surgery versus the more common, open procedure. Pain and hemorrhaging are reduced due to smaller incisions and recovery times are shorter. The key element in laparoscopic surgery is the use of a laparoscope, a long fiber optic cable system which allows viewing of the affected area by snaking the cable from a more distant, but more easily accessible location.
Specific surgical instruments used in a laparoscopic surgery include: forceps, scissors, probes, dissectors, hooks, retractors and more.
From Wikipedia
And yes, my uterus is much smaller than the one in that illustration.
So they cut a slit, put in a tube, and blow some carbon dioxide in. Yes, so many snide remarks being filtered right now.
Then a few more slits, one has a camera, one a stapler or retractor or something, another a type of knife, etc. Several people would be controlling the instruments, there would be a monitor or two showing the inside view, and the surgeon running the show. At the end of surgery they will attempt to suck out all the gas, any left over may cause shoulder discomfort for a couple of days after surgery. (Yep, it ‘tickles’ the bottom of the diaphragm and you have referred pain. The body is so fucked up.)
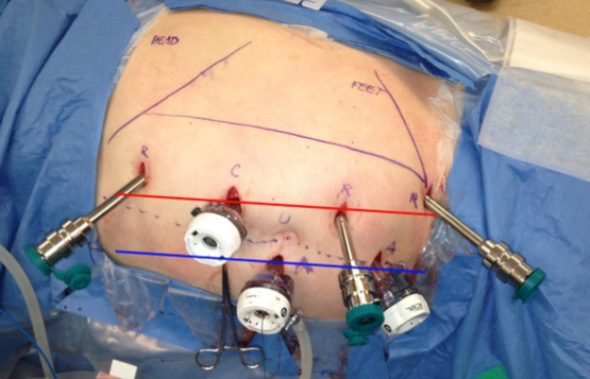
Click for a photo of a patient with said instruments
And then came da Vinci. This is the name of a surgical robot that aids in the surgery. da Vinci cannot and does not do surgery on its own, it is not that kind of robot. What it does do is control the instruments under the direction of the surgeon. The surgeon has complete control at all times. The robot filters out any hand tremors, magnifies the motions as desired, etc.
This is a great video explaining it all. There is about 1 second of insides near the beginning that does not really look like anything and should not typically be objectionable!
Click for an even better demo of the machine, but a good amount of internal body views!
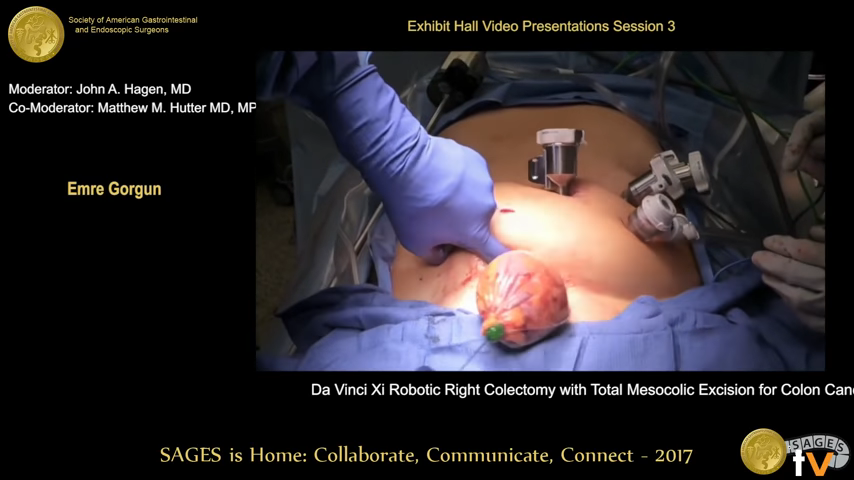
And, if you really are a sicko, here is the entire surgery I am having from the point of view of the camera that will be in my belly …
Click here at your own risk
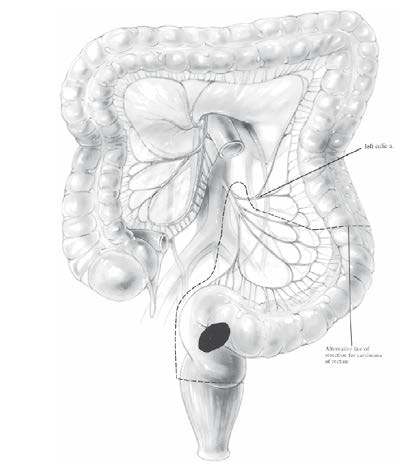
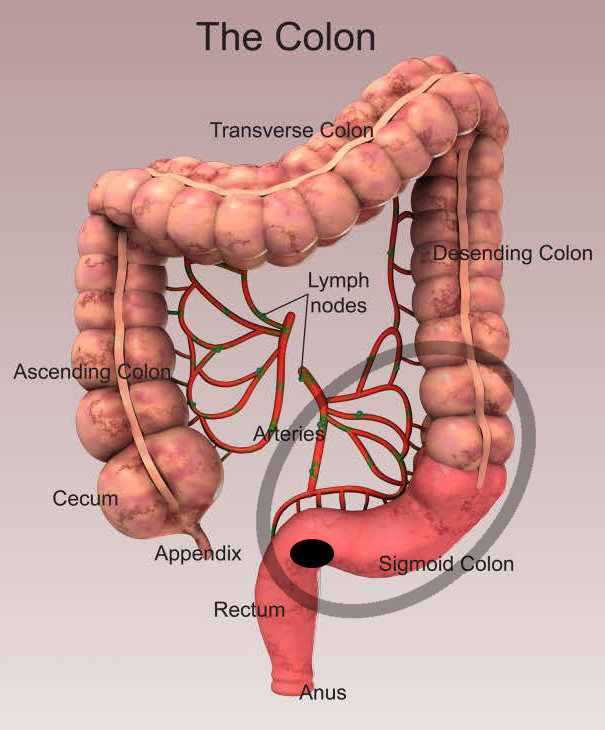
da Vinci Robot Assisted Low Anterior Resection with Diverting Loop Ileostomy
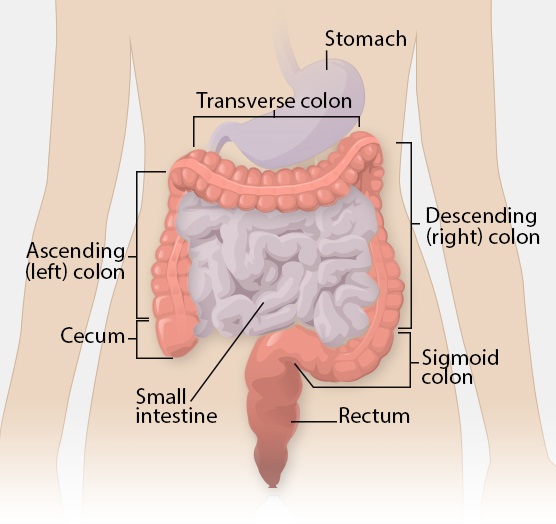
And if you are wondering how they get a foot of colon, with tumor, out of me?
Click here for a screenshot of how …
And now I must admit, I pine for the good old days, the days of my childhood, those days when surgery was done by the neighborhood barber, the days of yore.

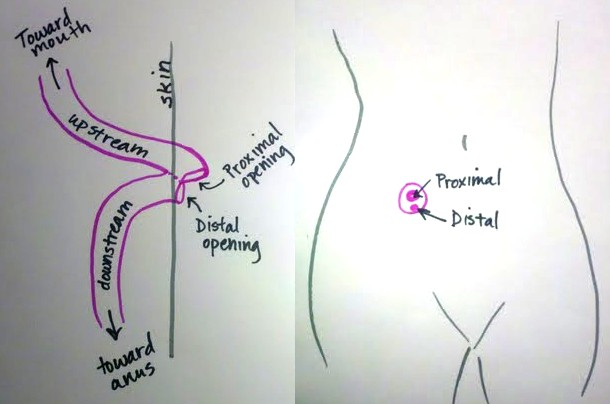
 And no, he did not pull a quarter out of his stoma … that is to show the size!
And no, he did not pull a quarter out of his stoma … that is to show the size!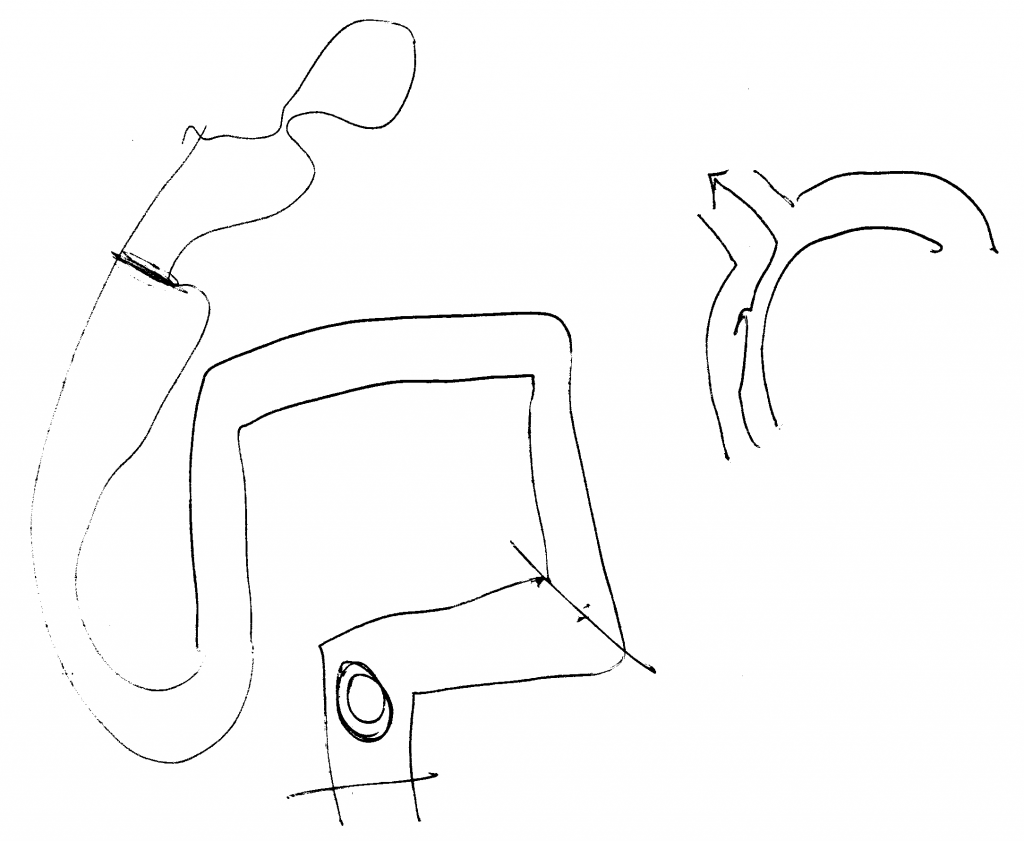










 What better cover to use when sitting around just shooting the shit with friends?
What better cover to use when sitting around just shooting the shit with friends?

No comments yet on this ↑ post, add yours (or read theirs)